Testing Australia's Medicare
One of the many issues fracturing the people of The United States is how to administer healthcare. Is healthcare a right? A privilege? Should we keep healthcare private, or should the government provide healthcare to all? The Australian government provides healthcare to its citizens. Time for an experiment! I decided that, on this trip, I would purposely test their healthcare system. Just kidding. None of this was on purpose. It all just happened. But I did get to experience Australia’s healthcare system firsthand.
To tell you this story, I have to divulge something I’ve kept mostly private for the last year and a half: I have cancer. It’s a blood cancer — not leukemia — called Essential Thrombocythemia (ET). ET is both genetic and non-hereditary, which seems contradictory. A spontaneous gene mutation causes ET (genetic), yet no one knows why the gene decides to mutate. But your parents give you no predisposition to it (non-hereditary). The mutation triggers your bone marrow to furiously churn out platelets, like the 1980s “Time to make the donuts” Dunkin’ Donuts commercials. The extra platelets clump together in your bloodstream like rival gangs in a prison yard, which can lead to blood clots. These clots increase your risk of stroke or heart attack. Perversely, the condition can also lead to excessive bleeding, as the platelets are so busy clotting with themselves at random places in your bloodstream that they don’t rush to heal a flesh wound or otherwise go where they’re needed. This article contains more information about ET.
ET is much less scary than other cancers, though. Typical treatments include blood thinners, like aspirin, to discourage blood clots from forming. Another treatment option is oral chemotherapy — pills — like hydroxyurea. This chemotherapy kills platelets to reduce the platelet count in the blood. Properly treated, patients can live a normal lifespan. Consequently, I feel a little sheepish mentioning my cancer, especially since my sister has battled (and just conquered!) the real kind — the kind where they chip pieces off you to biopsy, and then hack chunks off your body and fill you with poison through a port on your chest and then burn your skin with the heat of a thousand suns while your hair flees your head and you vomit in pain. And a coworker continues to battle this kind of cancer. I call mine a “baby cancer,” mostly don’t tell people, and invoke the “But I have cancer” card only when I want my wife or children to make me a sandwich (note: it never works).
My oncologists have been managing my ET with both hydroxyurea and daily aspirin for the last year and a half. I take my pills every day, get blood tests every three months, and meet with my oncologist to review the results. My platelet levels have been brought down from dizzying heights (over triple the normal range) to normal levels. Life moves forward. I deal with some fatigue and shortness of breath, since the hydroxyurea creates some collateral damage to red blood cells (the ones that carry oxygen). I also have more susceptibility to infection, as white blood cells also take some hits from the hydroxyurea. Still, my oncologist has been pleased with my progress.
About three months ago, I noticed what I thought were a couple bug bites on my lower left leg. Coincidentally, it’s the ankle that randomly swells, following no pattern I can discern. I blame my motorcycle accident that broke that ankle. I mostly ignored the bug bites, expecting them to heal on their own, until I noticed they’d lingered for about six weeks. Not connecting any dots, I went to my primary care physician (PCP) and said, “Hey, I was mowing the tall grass behind my back fence, and got these bug bites that aren’t going away.” She looked them over and prescribed some steroid cream to accelerate healing. A couple weeks later, the “bug bites” hadn’t shrunk. Instead, they’d turned red and inflamed. I went back to my PCP, who prescribed an antibiotic. The next day, I went to my regularly-scheduled oncology appointment and thought, “Hmm, maybe I should mention these bug bites.” Good call. I learned that, because hydroxyurea kills platelets, it can inhibit wounds from healing. Further, it can actually cause wounds like the ones I had on my lower leg. My oncologist had me stop taking the hydroxyurea immediately and began the process to refer me to a wound care specialist. My Australia trip loomed, though, so I didn’t have time to connect with the wound specialist before leaving. I did have time for one more blood test after a week without hydroxyurea, and my platelet count was 25% above normal range. My oncologist prescribed Eliquis, a blood thinner, to take along with my aspirin during this trip. I’d done all I could, felt fine, and was ready to go.
When I packed for my trip, I packed my aspirin, my Eliquis, and even packed my hydroxyurea in case I got a message from my oncologist to resume it. What I meant to pack as well was my inhaler, which I have for occasional use — mostly for pine pollen allergies — but I hadn’t used it in almost a year and simply forgot to put it in my backpack. It’s sitting in my top nightstand drawer. Cue the ominous music.
We left home about 7:30AM Wednesday, August 14th. We picked up Russ’s cat from Jakey’s house on our way to the airport. After a full day of flights and layovers, we crossed the United States and landed in Los Angeles. Wednesday night, we boarded the 15-hour flight to Melbourne. I’d say we flew through the night, but since we crossed the International Date Line we sorta flew through time. We slept a little on the flight — probably four or five hours — and landed in Melbourne about 6:30AM local time on Friday morning, about 33 hours after we’d left our house Wednesday morning. Determined to beat jet lag, we decided to stay awake until at least 8:00PM that night, so we’d adapt right away to the new time zone and make the most of our trip.
We cleared customs, hugged Russ and Jhett, and chattered away as we headed to their apartment in Point Cook, southwest of Melbourne. After a quick apartment tour, Jhett made us lattes on his Breville, which we sipped in their family room. Jhett left for school, and Sherry and I showered off the travel and dressed.
Have I mentioned that I’m allergic to cats? Russ and Jhett already had two cats, not counting the one we’d brought from the US (who was now sitting in quarantine), and I started to feel their effects. I’d taken a Claritin, but my eyes started itching and turning red. Russ banished me to their second-floor balcony. The itching subsided. Russ, Sherry, and I then left their place about 10:00AM and poked around the shops near their place. At 2:00PM, we checked in to the house we’d rented for the duration of our trip, a 10-minute walk from Russ and Jhett’s apartment. I sprawled on the couch and read my book while Sherry unpacked. At some point — I want to say about 4:00PM — I noticed that I was wheezing a little. Jhett arrived about 5:00PM and cooked salmon and risotto for dinner. My breathing was becoming more labored, so I took a couple Benadryl and sat down to eat. Breathing had become somewhat more difficult, though, so I couldn’t eat much and excused myself to our bedroom. I found myself wishing I’d remembered my inhaler.
My breathing became more difficult. Have you ever been drinking Coke through a straw that has a small crack in it? You suck in with full effort, but get only half the Coke you expected. That’s what my breathing felt like: I inhaled deeply, but only got half the air I expected. This differed from panting after going on a run or playing basketball. This had a desperation to it: a wheezing inhalation, then a brusque exhalation that almost crossed paths with the next inhalation. I struggled to find air. The pace of my breathing accelerated as I tried to get more oxygen. I wondered if I was having a panic attack, so I willed myself to slow the pace of my breathing and take extra-long, extra-deep breaths. My breaths were longer but not any more fruitful. My mind raced. I popped two more Benadryl. I wondered if this was a delayed effect from the morning around cats. I wondered if the couch I’d sprawled on in our rental was full of cat dander. I wondered whether my elevated platelets were giving me a heart attack. I wondered whether my double-whammy blood thinners were making my blood too thin to carry oxygen. I wondered if I’d picked up a particularly virulent strain of COVID on the plane that was ravaging my lungs. I knew I should have worn a mask, but 15 hours of muffled breathing and fogged glasses had seemed unbearable. I wondered if the flight had given me a pulmonary embolism. I’d worn compression socks on the plane, and made sure to get up and walk around every three hours or so. I mean, I didn’t think I was dying, but I was starting to entertain that possibility. I thought, “I’m most likely okay, but would feel pretty stupid if I did nothing and suffocated.” So when Sherry came in to check on me, and she saw how I was struggling, I only weakly protested when she said, “We’re going to the hospital.”
The closest hospital was Werribee Mercy Hospital, about a 10-minute drive from our rental. Russ and Jhett said their friend had recently spent six hours in their emergency room awaiting treatment. That didn’t sound attractive. We debated a few options, and my plaguing thought was, “What is this going to cost me?” When I spoke, it followed the cadence of a blacksmith’s bellows: pause while inhaling, wheeze out a few words while exhaling. Wheeze in, “I don’t,” wheeze in, “think that,” wheeze in, “need to,” wheeze in, “go to,” wheeze in, “the hospital.” They ignored me. I soon heard Russ on the telephone. He’d dialed 000, Australia’s 911. What was an ambulance going to cost me? “My dad can’t breathe,” he kept saying. “It’s not that,” wheeze in, “I can’t,” wheeze in, “breathe,” wheeze in, “it’s just,” wheeze in, “hard to,” wheeze in, “breathe.” I felt the conflict between accuracy and pedantry. I also knew I couldn’t die and put that guilt on my son.
Minutes later, an ambulance pulled into the driveway, lights flashing and siren whining. I noticed that the siren followed the continuous up-down pattern of US sirens, not the bing-bong, high-low whine of European sirens. Two paramedics appeared with a stretcher. Energetic, friendly, efficient. Both young women, I’d guess in their 20s or 30s. I think I climbed into the stretcher on my own power, and they strapped me in, wheeled me out, and loaded me up into the back of the ambulance. One drove and the other rode in back with me, asking me questions. I remember her dark hair and dark-rimmed glasses. She asked me lots of questions, but in a conversational way, like a getting-to-know-you speed date. “Do you know where you are?” “Austral-,” wheeze in, “ya.” “Do you know what day it is?” Ha! A trick question! “Friday,” wheeze in, “August six-,” wheeze in, “teenth.” I felt smug. “Have you had trouble breathing before?” “Not like,” wheeze in, “this.” Round and round we went, exploring my cancer, my cat allergies, my travels. I told her about my inhaler, which she called a “puffer.” She was competent and cheerful, doubling back when she needed more information, and had gathered my health story by the time we’d arrived at the hospital. They wheeled me into a hallway. They shoved a cannula into the crook of my right arm and clamped an oxygen probe onto my finger. An administrator asked me for my Medicaid card. The paramedic said I wasn’t a national. “Oh,” said the administrator, and asked me for a credit card and a signature. She explained that I was into this $670 for the ambulance ride, and that I’d get an email bill for anything else they did. I signed while thinking that, while $670 was cheap for an ambulance ride, I still wasn’t wild about paying it. My phone chirped with a notification from my bank: $444.68 to Werribee Mercy Hospital. I’d forgotten about the exchange rate between Australian and US dollars. That amount felt better.
They pulled up my shirt to expose my chest. Sticking leads all over my chest, they explained that they were doing an ECG, or what Americans usually call an EEG. Or maybe I have that backward. They said my “O2 sat” (oxygen saturation) was 90-91% — low, but not alarmingly so. They snaked an oxygen tube under my nose. They asked me if my chest hurt. They checked the wound on my leg and tested for diabetes. And they observed. I sat in the center of an awful lot of attention for a time.
Sherry, Russ, and Jhett had followed the ambulance to the hospital in Jhett’s Jimny. They weren’t allowed to follow me into the hospital. One person, they said, could wait with me in the waiting room, but since I wasn’t in the waiting room, they weren’t allowed in at all. They returned to Russ and Jhett’s place, pestering me for updates by text.
After about 20 minutes, I noticed two things: I was breathing a little easier, and the attention was drifting away. My EEG came back normal. A triage nurse came by and asked a few questions. My quandary: I was in that gray area where health has improved but not completely. Do you fudge a little so you don’t get dropped? Can you even trust your perceptions? Maybe I no longer teetered on the precipice, but was I still near the cliff’s edge? I tried to answer truthfully, skewing slightly in the direction of “I may feel better, but don’t abandon me yet.” The triage nurse left. And I waited some more in that hallway. Eventually, probably 20 more minutes, I felt completely fine. I breathed normally. No more wheezing. No desperation. Not only had the crisis passed, but even any gray area had vanished. I was as normal as I ever get. My EMT from the ambulance came back by, unhooked my EEG leads, unstrapped me from the stretcher, and told me to go to the waiting room. I asked if I should just go home. She said no, that staying to get fully checked out and discharged would be better. Here’s where my story turns.
I walked into a packed waiting room. Not many empty chairs, but I found one. I plopped down and texted Sherry. Someone asked me if I was in line. “I’m not in line,” I said, expressing my intent. “Oh, you’re in line,” someone responded, describing my reality. Apparently, the chairs were color-coded: teal was the line to talk to the front desk, navy was the sit-and-wait section. I relocated to a navy chair. I scanned the nearly-full room. A stoned guy was making Daffy Duck impressions, responding to each announcement from the PA system with a quack. He proclaimed the room was too hot, and took a poll of the people around him. He tracked down a worker and asked for a thermostat adjustment, and got denied. He then apologized to the room, repeatedly, for his failure. Someone else grabbed at his abdomen, near his groin. He kept moaning. He slid off his chair to the floor and continued to clutch and moan. He stood, limped to the center of the room, and sprawled on the floor, continuing to moan. A worker directed him back to a chair. He tried to explain about his pain, but she wasn’t swayed in the least. Stone-faced, she told him to get off the floor and sit down in a chair. I felt no judgment. This is their job: they triage people in pain all day, every day. They can’t afford to emotionally attach to everyone. My allegiance to my ambulance EMT faded. I had to get out of there. My health was fine. I was fine. Others deserved to be treated before me. I was travel-weary and couldn’t face six hours in this waiting room, hoping to rise to the top of the list to be seen.
I thought about approaching the front desk to tell them I was leaving. They looked like they would shoo me away and tell me it wasn’t my turn. I thought about just walking out, but I still had this cannula in my arm. I figured I could just slide it out, but wasn’t entirely sure of the repercussions. Can you really just yank out a cannula and slap a bandaid on it? I figured that Jhett, with his veterinarian training, would know and could perform this task. I texted him, and he expressed willingness with some misgivings. Apparently, birthing a calf and neutering a dog feels different from tending to a cannula on your boyfriend’s father. I realized that I wasn’t brave enough to just walk out of the hospital anyway, not sure of any legal or financial implications. By this time, my crew had returned to the hospital. Sherry came in and sat with me in the waiting room. Each patient had a one-person limit, so Russ and Jhett waited in the parking lot. I said, “Ok, if they haven’t called me in 10 minutes, I’ll just leave,” expressing a bravado that lay beyond me. After 15 minutes, I saw a nurse walk through the waiting room. I rushed to her, pointing to my cannula, and said, “Will you take this out? I’m fine. I’m leaving.” She nervously said, “Technically, we can’t hold you,” while simultaneously scanning her list for my name. She found it halfway down, steeling my resolve to get out of there. Again, she said that they couldn’t hold me, then said she’d have someone take out my cannula. She left, came back about five minutes later, and led me to a small room just off the waiting room. While I watched, hawk-like, she removed the tape from the cannula and slid it out. That was indeed all it took; I’ll know for next time. She held a cotton ball to the spot on my arm for a few seconds, then lifted it up. Blood pooled out from the injection site. I held my breath, knowing that my blood thinners would slow the clotting and willing my platelets to knit, lest she claim I couldn’t leave with so much blood flow. She pressed the cotton ball again, this time a bit longer, then taped the cotton ball in place. I waltzed out of the hospital, free to go home. We loaded into the car and drove home with all the windows down, despite the freezing air whistling in, so that no lingering cat dander on anyone’s clothes could choke me. Sherry showered again — the third time of the day — to expunge any remaining cat. Exhausted, Sherry and I went to bed in our rent-a-home, and Russ and Jhett went home.
I awakened in the night to pee and felt something pulling a little on my side. I probed my side with my fingers, and felt a nubbin poking out. Coincidentally, it protruded from the same place they’d poked a hole to drain my lung after the aforementioned motorcycle accident. In my fugue-like state, I thought the nubbin was related to that hole. I pulled up my shirt, looked down, and laughed. All the EEG stickers were still stuck to my chest. I waited until the morning to peel them off.
Here are my souvenirs from the hospital. The EEG stickers:

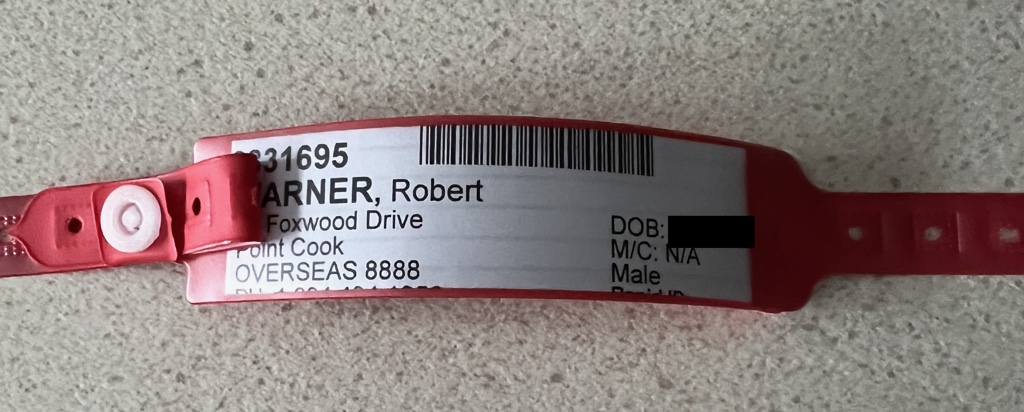
And my hospital bracelet:
What was the cause for my breathing difficulty? We don’t know. They told Sherry that it wasn’t presenting as an allergic reaction, but they found no evidence of an embolism, heart attack, or stroke. The most likely explanation: a combination of fatigue and cat exposure. Whatever the reason, I had no other breathing issues for the rest of the trip. Sherry and Russ banned me from entering Russ and Jhett’s apartment for the rest of the trip. Every time we walked somewhere, either Russ would walk next to me and command me to slow down, or Sherry would walk next to me and listen for my breathing. I’d put a good scare into both of them, but everything turned out fine.
The following Thursday, I had another Australian healthcare interaction. Remember the wounds on my leg? The redness, swelling, and pain returned. Sherry began pestering me to get it looked at. We did an Apple Maps search for “clinics” and saw one in the shopping center between our place and Russ’s, so we walked over. We walked into a clinic that was brand-new and modern, and asked to see a doctor about my apparently-infected wound. They said, sorry, we have no doctors here. Odd. What was the purpose of this clinic, then? We didn’t press the issue and left.
We found another clinic across the street from Russ and Jhett’s place. Sherry remembered that that’s the clinic Russ uses. We walked in and asked to see a doctor. They apologized and said they were booked for the day. Bracing myself to hear that the next opening would be in three weeks or more, I asked for an appointment. They offered me 8:00AM the next morning. I took it. The next morning, I arrived 10 minutes early, and the doors opened at 7:58AM. By 8:00AM, I was sitting with the doctor, showing her my leg. She probed for information, asking familiar questions about my health background as I explained about the ET and the hydroxyurea and my previous antibiotic. As with the paramedics, I was speaking to a professional: bright, competent, personable. She wondered aloud if the sore on my leg was a diabetic ulcer. Remembering I have all my blood test results on my phone, I launched the MyChart app and handed her my phone. She scrolled through all my blood test results while I idly wondered whether I’d first have to sign a HIPAA release form in the US. She clearly knew what she was looking at. After a few minutes, she concluded that my glucose numbers were fine, that I didn’t have diabetes, and she wrote me a prescription for an antibiotic. Cephalexin. She also performed a swab test on the wound, saying she’d call me with the results on Monday. Since I didn’t have an Australian phone number, I’d used Russ’s number on the intake form. She said that wouldn’t be a problem. Total cost of visit and test: $80. Again, I’d forgotten that the dollars were Australian. $54.10 landed on my credit card.
I walked to the chemist, which is what they call pharmacies in Australia. Direct Chemist Outlet. I handed the … chemist? Pharmacist? … my prescription, and they apologized and said it would take a few minutes to fill and asked me to take a seat. I sat down, noted the time, and started to play Spelling Bee on my phone. Four minutes later, they called my name. Four minutes. They charged me $9.99 for the box of pills, which converted to 6.76 USD. I took three pills a day for 10 days, and my infection cleared up.
How about the results of my swab test? I’ll never know. The clinic called Russ a few times, and they played a bit of phone tag. Whenever they connected, they’d schedule a time for the doctor to call him to give the results, but the doctor never called. I didn’t worry too much, knowing I’d be back in the US and will soon see a wound care specialist.
One last interaction with the Australian healthcare system. The morning after we arrived in Australia, Sherry awoke with a headache. That became a stuffy nose as the week progressed, and she started taking Sudafed. I started to get the sniffles as well, so began taking Sudafed as well. Russ had had the flu the week before we arrived, so we figured he’d passed something on to us. Not the case. At dinner on Thursday, Sherry noticed that she couldn’t taste her fancy passionfruit soda. Warning bells clanged. We went to the chemist and bought COVID tests. Both Sherry and Russ tested positive, though Russ’s “positive” line was faint. The next day, I tested positive for COVID. Jhett was negative. We lost our weekend plans — a footy game and our Great Ocean Road adventure — to COVID. We spent the weekend in quarantine. Based on timing of the symptoms, we figure Sherry and I got COVID on the plane, and then passed it to Russ. We never saw any doctors for the COVID, relying instead on at-home COVID tests to guide us. We ended up buying two boxes of COVID tests from the chemist, five tests per box, about $20 per box. Even though shopping for COVID tests is a bit like shopping for maxi pads or condoms — the cashiers probably don’t care, but you feel a little exposed — I was glad to see that the chemist had plenty of tests for sale.
Do you have any conclusions about Australian healthcare, or whether public or private healthcare is better? I don’t. I had mostly terrific interactions with Australia’s healthcare system, with a few negative ones (the waiting room at the emergency room, no results from my swab test). This mirrors my experience with the US healthcare system — I’ve seen a lot of doctors, and those doctors a lot, over the last 18 months. My doctors have treated me meticulously, promptly, expertly, and with great concern throughout. I still haven’t heard from the wound care specialist after four weeks, though, and will have to chase that referral. Healthcare costs are lower in Australia, but their taxes are higher. And my few anecdotes don’t constitute complete data. My experiences, though, tell me: healthcare professionals in both countries are qualified and engaged. Healthcare is expensive, whether through premiums and copays or through taxation. And healthcare generally is a difficult problem. Finally, I need to get my leg looked at, soon! And if you’ve read this far, Mom, I’m sorry I didn’t tell you about the ambulance ride sooner. I know you’d have jumped on the next plane to Australia, whatever the fare, with my puffer in hand.
Update: Sept 13, 2024: A few nights ago, Sherry was experiencing some health issues. Time to retest US healthcare. Here’s a timeline:
- 7:30pm — Decide to go to the Emergency Room.
- 8:15pm — Check in at Emergency Room. Waiting room is sparsely populated, but they tell us we just missed a mad rush of people who are now sitting in treatment rooms, getting care.
- 10:45pm — Sherry’s pain has somewhat subsided. We’ve spent 2.5 hours watching people arrive, check in, and get called back. They’ve clearly triaged Sherry down the list. In tears and exhausted, she pulls off the hospital bracelet and tells the front desk to check her out. Apologetic, the staff talks her out of leaving, assuring her that a room was nearly ready.
- 11:00pm — Two more people have been called back. The “nearly ready” room has obviously been given to someone else. We try to leave again, and again they convince her to stay.
- 11:10pm — We’re taken back to a room. They insert a cannula in Sherry’s arm but hook up no monitoring of any kind.
- 12:10am — The doctor arrives, asks some questions, pokes and prods, and says they want to do some imaging.
- 2:00am — Someone comes and takes Sherry for a CT Scan. Everyone else has been kind, concerned, and engaged. This person is none of these, but rather is curt and irritated.
- 2:10am — Sherry returns from CT scan.
- 4:00am — Doctor returns. Scan is clear. Doctor imparts instructions.
- 4:15am — We are discharged, get in our car, and drive home.
Scorecard:
- Total time: 8 hours
- Total tests: 1
- Total monitoring: 0
I’m not criticizing. I’m sure everyone was working diligently, and that they reasonably maximized time and resources to see patients in the best order possible. In my experience, though, both the public and the private healthcare models have comparable challenges and delivery schedules.
